

Ravi Raichur
Data Liquidity In Healthcare Drives Patient Outcomes And Satisfaction
What is Data liquidity?
Interoperability has been around for quite some time in the healthcare industry. Interoperability in a healthcare set up is relevant when we have multiple health IT systems talking to each other. Health IT experts, Governments have been campaigning hard for pushing EHRs and Meaningful use for better interoperability. Of late, EHR’s inability to communicate effectively with other systems has been a big concern for healthcare industry. However, the new paradigm of data liquidity could just solve the problem.
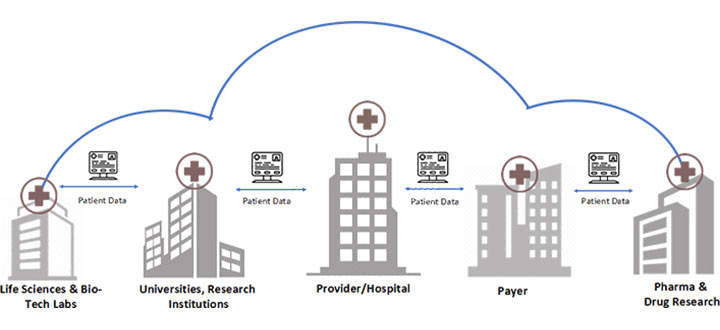
Data Liquidity, the new kid in the block has been discussed at length in recent health IT meet-ups, events and conferences. Put simply, Data liquidity ensures that actionable, relevant and accurate patient data is available at the point of care to the right caregiver, at the right time. It is also the ability of an electronic health IT system to communicate with various systems in a hospital. Data liquidity promises data flow along with the patient wherever it’s needed.
Interoperability vs Data Liquidity
Though at first glance, Interoperability and Data Liquidity appear to be synonymous. Interoperability need not necessarily include data liquidity. For e.g. there could be a health IT system (System A) that cannot accept few patient data points, instead it pulls data from a static form or a standalone report. This makes the data localized to “System A” and limits the usage of this data from downstream applications and systems. Meanwhile, data liquidity ensures interoperability of the data with downstream applications.
- Interoperability is a paradigm where a handshake happens between two different IT systems. For. E.g. a patient schedule instruction going from a scheduling system into a hospital EHR may include an HL7 ADT – admit/discharge transfer. A radiology report getting logged into an RIS through a standard interface that allows the report to be filed. While interoperability is focused on addressing data aggregation and availability, the healthcare industry has the task cut out in showing marked improvements in care quality and patient outcomes.
- Data liquidity is a phenomenon in which patient data entered once is consumed by downstream applications/systems and other users in the same or different location, at varied intervals of time. For e.g. the data from patients or a specific demography group declaring allergy conditions, types that they are prone to, could be used to pull reports and analyze the percentage of patients allergic to a foreign substance in a population.
In addition to a platform for connecting, storing, archiving, viewing and exchanging patient information, data liquidity could be progressively leveraged for analytics, personalized medicine, pay-for-value management, care coordination and management, population health management, and compliance.
Data Liquidity Use cases
The next gen personalized medicine and care delivery use cases highlighted below, depict the tremendous impact that data liquidity could have in improving research, care delivery, patient outcomes and health:
1. Research Management
Data is the new currency for business transformation and innovation. Researchers in various disciplines including basic science, life sciences, drug discovery, pharma, clinical, and behavioural health need access to relevant data to move forward with their research. A detailed analysis of molecules, life style, genotyping, clinical, laboratory, sequencing data helps researchers identify populations at risk, predict a patient’s response to a therapy, provide prognosis and risk analytics, and aid in developing new drugs.
2. Clinical Trials and Research Management
Researchers could analyze and screen patient data obtained from physicians in real time, thus enabling them to identify and qualify eligible patients participating in clinical trials. This would help researchers assess and identify the prevalence of specific mutations or combinations of mutations, and then identify the associated patients and their physicians for further follow up. Clinical Researchers need to manage a variety of data ranging from EHR, Laboratory, Patient reported outcomes, Diagnostic images, Telemedicine, and other external data sources. Clinical Trials Information system need to include an array of functionalities from study, design, patient recruitment and management, data integration and management, data liquidity to various compliance related reporting. Data liquidity can be achieved through a robust information platform, to aggregate data and store in specially designed data lakes, to serve the complex needs of modern research, support and collaboration.
3. Population Health Management
Leveraging data liquidity, Clinicians and Physicians with an access to demographic cross-sectional, trending, performance and life style data could arrive at clinical decisions swiftly. Clinicians will be able to more rapidly and accurately identify patients at risk for chronic disease and poor outcomes. Thanks to data liquidity at the point of care and decision making.
What is the Future of Generative AI in DevOps?
DevOps automation workflows are continually improving, and Generative AI is becoming increasingly important. It excels at understanding human language and providing responses that sound natural. This makes it highly beneficial in automating a wide range of DevOps tasks, from managing computing processes to troubleshooting issues.
By utilizing Generative AI, DevOps teams can reduce manual workload, minimize errors, enhance communication and collaboration, and save time by delegating tasks and understanding human language.
Generative AI’s value in DevOps is growing as it is capable of performing numerous functions. Organizations seeking to enhance their operations can leverage Generative AI as an essential tool. When seamlessly integrated into DevOps, Generative AI can streamline operations, improve efficiency, and adeptly manage the rapid changes in today’s technology landscape.
4. Closed care delivery circle
A connected, collaborative network of patients, providers and payers fosters trusted relationships, thus providing maximum value. Patients through mobile and digital health apps get real-time access to pertinent information regarding their health conditions and seek expert advice tailored to their needs. Patients will be able to share clinical information from their provider network to electronic health record portals, enabling data integration, storage and viewing by qualified physicians to enhance patient care, safety, communication and education. Patients could be given an option to view and choose to submit their data to researchers/clinicians, to aid in research.
5. Healthcare Systems innovation:
Pharma companies can query massive amounts of phenotypic and molecular data to examine patient populations for clinical trials recruitment. The molecular, clinical, laboratory, and imaging data powers research institutions to eloquently bridge the gap between clinical treatment and clinical trials data, thereby helping drug companies keep a track on their product performance (pre and post-marketing).
Conclusion
Data liquidity has grown to become a strategic imperative with its ability to export, aggregate and analyze the patient data to drive value based incentives, population health, clinical research and trials management.
According to a McKinsey report, Predictive modelling, Statistical Tools, Methods/Algorithms (for clinical trial design), Clinical trials data analysis, Personalized medicine, Disease registries analysis are identified as five key levers that will improve R&D productivity add create value worth $100 B. To realize this, data liquidity must be leveraged intelligently and meaningfully.
Interoperability is key, but there is more to data liquidity than a simple health information exchange service. Structured data in healthcare can build a solid foundation on which services like clinical knowledge, analysis and informed decision-making thrive and add immense value. Next generation health IT systems should have an integrated data liquidity piece, in addition to interfaces, interoperability and health information exchange. An innovation ecosystem comprising path breaking solutions in the areas of chronic care, data liquidity, worker productivity, and provider-payer payments at the systemic level are sure to transform healthcare in the coming days.
Related Insights


Artificial Intelligence in Healthcare: Saving Lives and Care

AI-Powered Personalization in UX: Enhancing User Experience in Healthcare



